What is Asthma?
Asthma is a condition in which your airways narrow and swell and may produce extra mucus. This may make breathing challenging, bring on a coughing fit, cause wheezing when you exhale, and shorten your breath.
Various triggers can cause varied symptoms in different cases of asthma. Allergens, such as pet dander or dust, are frequent triggers. Additionally, some persons get asthma symptoms in response to particular diets or physical activity. In many cases there is hereditary link with family members being along having history of allergic symptoms like Asthma, allergic rhinitis and urticaria
Each year, Asthma is responsible for more than 400,000 hospital admissions and 1.8 MILLION visits to the emergency room. India has a 3 percent (30 million patients) asthma prevalence, with a frequency of 2.4% in people over the age of 15 and a range of 4–20% in children. WHO estimates that 235 million people worldwide suffer from asthma, out of which 15–20 million people are from India. More common in female adults than male adults. Around 9.8% of female adults have asthma, compared to 6.1% of male adults. It is a leading chronic disease in children.
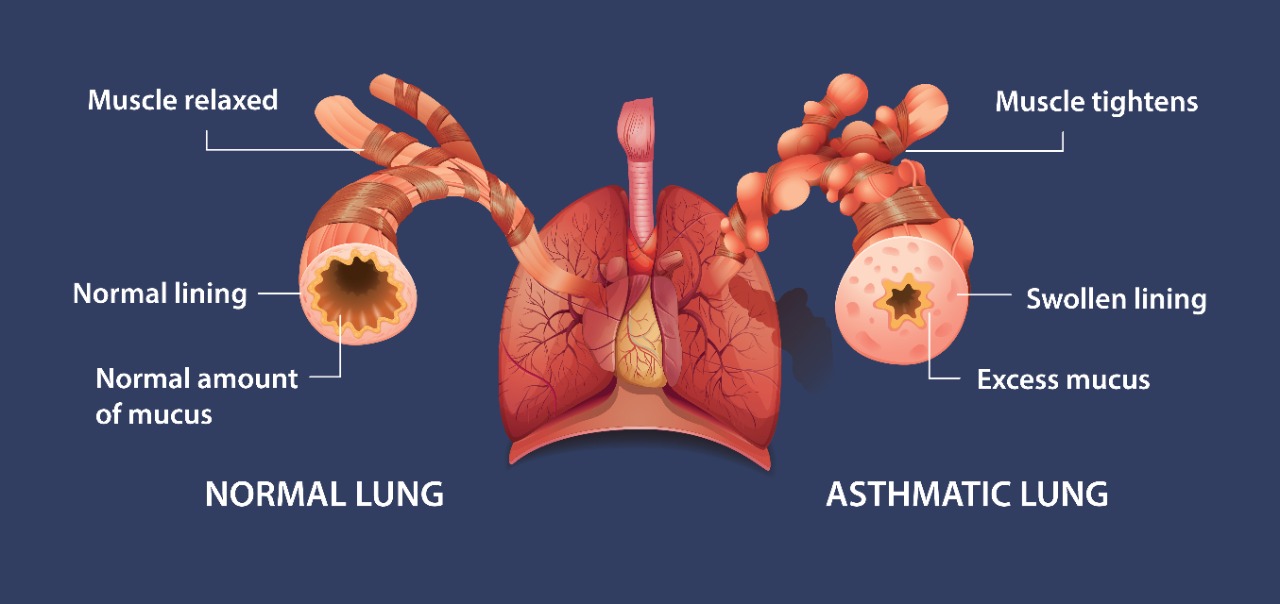
What happens to your body when you have an asthma?
The interior of your airways swells significantly more when a trigger occurs. As a result, there is less room for air to enter and exit the lungs. Your airways' encircling muscles may also get tight, which will make breathing even more difficult. When such occurs, it is referred to as a "attack" or asthma "flare-up."
Symptoms include Shortness of breath, Chest tightness, Wheezing, Coughing and Trouble sleeping. For some people, asthma signs and symptoms flare up in certain situations: Exercise-induced asthma, which may be worse when the air is cold and dry. Occupational asthma that are triggered by workplace irritants such as chemical fumes, gases or dust. Allergy-induced asthma that are triggered by airborne substances, such as pollen, mould spores, cockroach waste, or particles of skin and dried saliva shed by pets (pet dander).
Asthma in children
Asthma is diagnosed in children as young as infancy. Although it might be challenging to diagnose, asthma in children can be just as dangerous as it is in adults. Common symptoms of asthma in children include- rapid breathing periodically, chest tightness, chest pain, tiredness and/or less energy to play because of poor sleep, coughing and wheezing that worsen with a cold or flu, coughing spells, wheezing or a whistling sound when the child exhales, shortness of breath.
Allergies, exposure to cigarette smoke or other air irritants, and obesity are frequently associated with asthma in youngsters. Usually, it runs in families.
The majority of asthma drugs used to treat adults and older kids can also be used to treat asthma in younger kids.
Asthma levels of severity
Asthma changes over time in response to triggers. That means your level of severity can go up or down at any time. This is why it is so important to keep monitoring and managing your asthma—even when it seems to be under control.
Inflammation vs Bronchospasm
How to differentiate between Inflammation and Bronchospasm.
Inflammation- A defining feature of asthma is inflammation. The lining of the airways thickens and swells as a result of inflammation. As a result, there is less room for air to pass through. In order for the airways to open, the aim of medication (often anti-inflammatory drugs) and treatment is to lessen or completely eradicate the underlying inflammation.
Bronchospasm- The term "bronchospasm" describes the contraction of the muscles that line the airways' outside. Additionally, this makes the passageway for air to pass through smaller. Treatment and medicine (often bronchodilators) aim to either prevent or induce muscular relaxation so that the airways can open.
Types of Asthma
The 3 main categories of Asthma are mild, moderate and severe persistent
Today, phenotypes are used to study Asthma. These observable qualities or characteristics come about as a result of the way your genes and environment interact. Biomarkers—clinical, genetic, and environmental responses—are used in a classification system for asthma. Utilizing this technique has the benefit of allowing you to forecast how your body will react to certain therapies.
The phenotypes of Asthma-
Type 2 Inflammation
A) Allergic Asthma: Asthma that is brought on by allergens like pollen, pets, dust mites, etc is known as allergic (or atopic) asthma. Around 80% of persons with allergic asthma also have a concomitant illness, such as hay fever, eczema, or food allergies.
B) Eosinophilic Asthma: When eosinophils in the bloodstream increase abnormally, it results in eosinophilic asthma (e-asthma). White blood cells called eosinophils are one type that naturally encourage inflammation to fight sickness. Airway inflammation can result from having an excessive number of eosinophils.
Non-type 2 Inflammation- Non-allergic asthma, or non-atopic asthma, is a type of asthma that isn’t related to an allergy trigger like pollen or dust, and is less common than allergic asthma. The causes are not well understood, but it often develops later in life, and can be more severe.
Molecular Targets of Severe Asthma -
Most asthmatics, between 5 and 10 percent, suffer severe asthma. That typically signifies that their asthma is not under control despite receiving various medications. They might experience greater daytime and nighttime symptoms, flare-ups, hospitalizations, and significant lung damage.
In the type 2 inflammatory pathways, these molecular targets called as Biologicals/ monoclonal antibodies are used
How to take your Asthma Medications
The majority of asthma drugs are inhaled using an inhaler and are available as sprays or powders. The drug enters the lungs' airways when you inhale it, where it is most required. Metered-dose inhalers, sometimes known as MDIs, or Dry powder Inhalers called as DPI’s are the most popular kind of asthma inhalers.
Inhaled medicine is the best form of treatment due to various advantages:
- The drug directly reaches the lung and so the action is immediate within few minutes
- Minimal doses goes to other body parts and hence the side effects are very minimal
- The drug dose is very less (there are microgram/mcg) as compared to tablets whose doses are in milligram/mg
- There is no addiction potential in inhalers as against the popular myth that it can be additcive
A nebulizer can be used to administer medicine to people of all ages, including little children. This device creates a mist of liquid medication that can be inhaled gradually over a 10- to 15-minute period.
No matter what kind of inhaler you use, it's crucial to ask your doctor or pharmacist to demonstrate how to hold the device in front of or within your mouth and how to time your breaths with the spray.
Numerous patients misuse their inhalers, according to studies. They don't receive the full dosage of the drug as a result. The spray must be inhaled slowly enough to allow it to enter your lungs deeply while still rapidly enough to prevent it from touching your tongue or face.
Many people, especially kids, struggle to appropriately inhale from an MDI. Using a valved holding chamber (VHC) or spacer is a typical fix. These gadgets are simple to use and enhance drug administration to the lower airways. They help lessen thrush (candidiasis), a common side effect of drug administration, and hoarseness (dysphonia). A one-way valve on a VHC that you attach to an MDI enables you to spray.
Managing your Asthma
The symptoms of Asthma may fluctuate over time and come and go. An Asthma strategic treatment plan is a crucial component of your overall asthma care strategy. Together with you, your doctor will develop an asthma treatment plan that will include the medications you should take and when. Additionally, it will detail what you should do to stop symptoms and handle flare-ups. The Action Plan will provide information on the medications you should take, together with dosage and frequency recommendations, for both routine care and in response to flare-ups. Although managing your asthma may first seem like a lot of work, making these changes to your daily routine can help you lead a normal life.
Coping with an Asthma Attack
Early detection of an asthma attack's signs and symptoms may help to stop it from occurring. Additionally, it's important to be aware of the warning signs and symptoms of less severe asthma attacks, which include: coughing, sneezing, itchy throat, tight chest, wheezing, shortness of breath, waking up at night, and rapid heartbeat.
These warning symptoms indicate that you are suffering a severe Asthma attack. Lips or fingernails turning blue, severe shortness of breath (gasping for air), difficulty speaking clearly (unable to speak in full sentences). Then visit the emergency room.
Get away from the trigger that started your attack. Take your quick-relief medicine as soon as you notice symptoms. Make sure to take your controller medicine as well. if wheezing and shortness of breath still persist, contact your health-care provider or get emergency help.
When to see an Asthma Specialist?
Even after following your regular treatment plan, you might still experience symptoms that interfere with your sleep or daily activities. In this case, a specialist visit (to an allergist or pulmonologist) may be necessary.
If you have ever experienced a life-threatening asthma attack. if after two to four weeks of treatment, you aren't improving. When asthma symptoms are severe and flare-ups are frequent. You have illnesses like severe hay fever, sinusitis, etc. that make your asthma more difficult to manage.
 Call For Appointment
Call For Appointment